Your Knee
- About Your Knee
- What Can Go Wrong
- Non-Invasive Treatments
- Knee Injections
- Arthroscopic surgery
- Personalized Partial and Total Knee Replacement
- Traditional Total Knee Replacement
- Revision Total Knee Replacement
- SHARED DECISION MAKING: PERSONALIZED PARTIAL KNEE*
- SHARED DECISION MAKING: PERSONALIZED TOTAL KNEE*
- SHARED DECISION MAKING: TRADITIONAL TOTAL KNEE*
*A shared decision making module must be completed by all patients undergoing surgery by Dr. Martin
.
About Your Knee
The knee is the largest and one of the most complex joints in the human body. It is what is known as a “hinge joint.” It is made up of three bones: the lower part of the thigh bone (femur), the upper part of the leg bone (tibia), and the kneecap (patella). The ends of the bones are lined with a spongy material called joint cartilage which cushions the joint. There are also two meniscal cartilages which help protect the joint cartilage. There are numerous ligaments (bands which connect the bones) and tendons (bands which connect muscle to bone). There are three parts to the joint (the medial, lateral, and patellofemoral joints).
Figure 1. Shows a healthy appearing knee joint and its three parts

.
What Can Go Wrong
The knee joint is a weight bearing joint and feels the force of 4 times the weight of the body with normal daily activity. The joint is surrounded by strong muscles which work to move and support the joint. The knee is so important in helping us walk, run and jump it can interfere with our quality of life and ability to do the things we want or need to do when it is not functioning properly.
Because the knee is so complex, you can imagine there is a lot that can go wrong. The following are the most common reasons we see people presenting with knee problems:
- Osteoarthritis: this is a mechanical condition where the joint cartilage wears out and the bone rubs against the bone
- Inflammatory arthritis: there are multiple diseases which can cause inflammatory arthritis including rheumatoid arthritis, psoriatic arthritis, gout, and many others. The common factor here is that there is something systemic going on leading to damage to the joint.
- Meniscal tears: these are tears in the rubbery discs that sit between the ends of the bones on the inside (medial) and outside (lateral) parts of the knee.
- Patellofemoral pain/Chondromalacia: This is a disorder, common in runners and people who use their knees a lot, where the cartilage behind the kneecap gets irritated.
- Trauma or Microtrauma (includes sprains, strains, fractures, ligament and tendon ruptures: this can include minor injuries up to severe fractures and treatment options vary greatly depending on the cause.
- Other: Other less common serious things like tumors, nerve and vascular issues can cause knee pain so symptoms should never be ignored and should always be evaluated by a physician.
Fig 2. Shows an arthritic knee

For more information on the knee from the American Academy of Orthopaedic Surgeons visit: http://orthoinfo.aaos.org/menus/leg.cfm
Non-Invasive Treatments
Surgery should be considered a last resort. There are some basic things which should always be tried prior to considering surgical intervention. These include:
- Weight Loss (if needed): The knee joint sees the force of 4 times the weight of the body with most normal daily activity. So if you are carrying around 50 extra pounds, that is felt as 200 pounds of ADDITIONAL pressure on the joint. Lose the weight, and the joint will feel better. Even if it doesn’t, you will be in better health, feel better about yourself and be a safer candidate for surgery. *always consult a physician prior to changing diet/attempting weight loss.
- Exercise: Numerous studies have demonstrated the beneficial effects of exercise for your knees. Strong muscles can support the joint and take pressure off. They can also help you walk and function better. Movement in the joint is important to keep it from getting stiff. Click here to print a knee conditioning program: http://orthoinfo.aaos.org/PDFs/Rehab_Knee_6.pdf *always consult a physician prior to starting any new exercise program
- Medications: Numerous medications, including acetaminophen (common brand: Tylenol), anti-inflammatories (common brands over the counter: advil, motrin, alleve, common brands presecription: Celebrex, Voltaren, Mobic), and tramadol (common brand: Ultram) all can be effective in controlling pain and symptoms associated with knee problems. Medications, even over the counter, can be associated with significant risks though and you should always consult with a physician prior to utilizing.
- Supplements: Several supplements, although controversial, possibly may alleviate the symptoms of knee arthritis and pain, with less of a risk than traditional medications. These include glucosamine sulfate (http://www.nlm.nih.gov/medlineplus/druginfo/natural/807.html) and Tumeric/Curcumin (http://www.nlm.nih.gov/medlineplus/druginfo/natural/662.html)
- Topical treatments: Numerous topical treatments may temporarily help including menthol based products, capsaicin, and others. Although not cures, these treatments can help alleviate pain, without risking the potential side effects of systemic medicines.
- Support & Compression sleeves/bracing: In the knee, there can be a role for support sleeves and occasionally for external bracing depending on the circumstances.
Knee Injections
Currently, Knee injections are a way to alleviate symptoms and possibly delay the need for surgery. Injections to do not cure arthritis. Numerous substances can be injected including:
- Cortisone: this is a powerful anti-inflammatory injected right into the joint. It tends to work quickly with patients experiencing relief usually within a week. The time in which the effects last are variable, but a good result is considered to be 3 months or more. Too much cortisone and local anesthetic injected into the joint can be counterproductive. For info on cortisone injection visit: http://www.drugs.com/pro/depo-medrol.html
- Hyaluronic Acid: This substance is FDA approved for and commonly used in the knee. It does not cure arthritis or regrow cartilage. It may lubricate the joint and have some anti-inflammatory properties. They are controversial and some recent studies have indicated they may not work as well as previously thought. It definitely does not help everyone. In Dr. Martin’s experience for every three people injected one gets significantly better, one gets somewhat better, and one has no benefit. They are generally safe, although there can occasionally be side effects. Dr. Martin uses two of these products which are made in the lab (there are other’s that are made from rooster combs and parts, which he generally does not use because of seeing more adverse reactions). For further info on the hyaluronic acid Dr. Martin uses please visit the manufacturers sites: a. http://www.euflexxa.com and b. http://www.orthovisc.com
- Platelet Rich Plasma (PRP) and Stem cells: These so called “biologic” treatements are relatively new and untested. There is little science to support their use at this time and they are not covered by insurance. There is no convincing evidence that they alter the course of arthritis or regrow cartilage. Dr. Martin continues to follow the evidence on these prior to recommending their use.
Arthroscopic Surgery
Arthroscopic surgery is a true “minimally invasive” form of surgery where several small incisions are made and instruments used to perform surgery within the knee.
Figure 3: Illustrates portals used in arthroscopic surgery (Image borrowed with permission from: Education4Knees. Star Group Publications 2014)

While arthroscopic surgery can be of tremendous benefit in a healthy knee with a damaged piece of meniscus cartilage or torn ligament, more and more evidence is coming to show that as the knee degenerates (which happens in most people after the age of forty) this surgery should probably be avoided. Individual cases should be discussed with an orthopedic surgeon.
.
Personalized Knee Replacement
Dr. Martin believes strongly that people should only pursue surgery as a last resort. His new book, Education4Knees, tells people everything they need to know to potentially delay the need for or avoid surgery. Despite best efforts to avoid surgery will be required for some. Fortunately, having completed all the appropriate steps to avoid surgery will help ensure the best possible outcome with surgery. The condition a patient is in going in to surgery has a lot to do with their result with surgery.
Traditional total knee replacement, where the joint is replaced with metal and plastic components which come in several different sizes, has been performed for about 40 years now with good success, however there is room for significant improvement. Studies both in the US and Europe demonstrate that from the patient’s perspective, about 1 in 5 patients who undergoes traditional total knee replacement is not satisfied with their outcome.
Figure 4 shows results of existing studies demonstrating patients not satisfied after traditional total knee replacement.

Dr. Martin also realized that many people who underwent traditional total knee replacement, despite everything going well without complications, were not satisfied. Patients are often dissatisfied because of persistent pain or because the knees do not feel natural. Because of this he believes “cautious innovation” is required. We know from studies that implant size is important. Studies have demonstrated that an implant being to big by just three millimeters (a very small amount) can double the risk of persistent pain after surgery. Because traditional implants are not shaped like a persons knee, it generally does not feel like the patients own knee. No surgical technique or procedure will satisfy 100 percent of patients and no surgery will have perfect outcomes, but that doesn’’t mean we shouldn’t strive for the best outcomes possible.
Because of this, using shared decision making, Dr. Martin began to inform patients of personalized partial knee replacements in 2010 and personalized total knee replacements in 2011. People come in various shapes and sizes…….and so should their knee implants.. Conformis, a company in the Boston, Massachusetts area was founded with the idea that modern imaging technology and manufacturing techniques can be utilized to create better implants. Each implant is customized and individually made for the patient. In addition, all the instrumentation to help the surgeon place the implant is also made specifically for the patient. This allows the surgeon to implant the device correctly, with a less invasive surgical technique (no hole is drilled in the thigh bone and less bone is removed compared with traditional implants). Dr. Martin has one of the world’s largest series of personalized knee surgeries and is active in studying and presenting his data worldwide. Personalized implants have been utilized widely at many of the most prestigious institutions in America and Europe.
Video 1. Watch this video to learn more about ConforMIS technology
Dr. Martin believes that when it comes to surgery, never perform a bigger surgery than is needed. NOT EVERYBODY NEEDS A TOTAL KNEE REPLACEMENT! Because a CT arthrogram can be obtained as part of the process to make the patient specific implant, the knee can be investigated further. Sometimes if only one or two parts of the knee are damaged, than only part of the knee needs to be replaced. To better understand this watch this discussion featuring Dr. Martin on a surgeon panel (Dr. Martin’s explanation begins 6 minutes and 16 seconds into this video):
http://www.orlive.com/conformis-inc-/videos/section-iii-patient-selection-24-46-
Download a brochure explaining customized partial and total knee implants:
Click here
Personalized Partial Knee Replacement
For patients who are found to have damage in only 1 or 2 out of the three parts of their knee there are numerous compelling reasons to consider a partial knee replacement:
- Less invasive surgical technique
- No muscle cut
- Minimal bone remove
- Less trauma to the body
- Potential for less medical risk
- Potential for less painful recovery
- Pain varies from patient to patient, but generally is less than total knee replacement
- Potential for quicker recovery
- Typically done as outpatient surgery with quick return to a normal life
- Typically better range of motion
- Knees generally bend easier with little physical therapy required
- Typically a more “natural” feel
- Most people with a personalized partial knee say it feels “natural”
- Doesn’t burn bridges for future
- Nobody ever wants a second surgery, but the fact is that with either partial or total knee replacement there are no guarantees
- If a partial knee fails or the rest of the knee becomes arthritic, it can typically be converted to a total knee
- If a total knee is performed rather than a partial knee and the patient is not happy with the outcome, you can never turn back to a partial knee
The potential downsides of partial knee replacement are:
- Parts of the knee are left behind that could become arthritic and painful down the road leading to potential need for further surgery
- Some studies have shown a higher early failure rate with partial knees versus total knees. However, recent studies with modern knee designs have demonstrated survival approaching total knees at 10 to 15 years of follow up.
Video 2: To watch an animation of a personalized partial knee, see below:
Video 3: To watch a cadaver teaching video of a personalized partial knee by Dr. Martin, see below (caution: this video is for surgical education and contains graphic surgical footage which may not be suitable for some. Watch at your own discretion)
For more information on ConforMIS Personalized Partial Knee Replacement you can download the following brochures or visit www.myconformisknee.com:
English: http://library.constantcontact.com/download/get/file/1111349463869-
111/MK02529AC_Patient_PKR_Brochure.pdf
English Frequently Asked Questions: http://library.constantcontact.com/download/get/file/1111349463869-
112/MK02528AD_PKR_FAQ.pdf
Spanish:
Personalized Total Knee Replacement
For patients with significant damage to the knee that are candidates for total knee replacement there are compelling reasons to consider a personalized total knee replacement:
- PreNavigated, single use instruments for the surgeon
- Instruments are made specifically for the patient
- Helps surgeon align the knee without using time consuming and somewhat unreliable convention instruments, computer navigation or robotics
- Instruments are used only for you and then discarded (unlike traditional knee instruments which are re-used and must go through sterilization process for each case
- Less surgical trauma
- No hole drilled in femur
- Less bone removed (25% on average)
- Less blood loss and swelling
- No hole drilled in femur
- Implant covers all cut bone
- Leads to reduced blood loss and swelling
- Minimal risk of transfusion (1% compared with 10 to 20% for traditional total knee replacement)
- Potential for less post-operative pain
- Less bleeding and swelling typically leads to less pain
- Potential for a quicker recovery
- Less pain typically leads to a quicker recovery
- Potential for less of a chance of persistent pain
- Customized implants have less of a chance of irritating soft tissues
- Potential for a more “natural” feeling total knee
- By recreating the normal anatomy, the hope is that the knee will feel more natural. Some early data has demonstrated this (see Current Research)
The potential downsides to a personalized total knee are:
- Lack of intraoperative flexibility
- Since the system is very conservative, if more damage is found than expected there is a chance the technique may not be possible
- No long term follow up
- Data is only out to three years and early failure rate is as good as or better than traditional total knees
- No data beyond this is available
- Many existing designs traditional total knees have data over greater than 10 years, but many of these designs are being phased out in favor of newer implants that come in more shapes and sizes
To watch an animated surgical technique video of the iTotal, see below:
To watch live surgery of a personalized total knee replacement using the ConforMIS iTotal G2 which Dr. Martin performed on ORLive , see below (caution:this video is for surgeon education and contains graphic surgical footage which may not be suitable for all viewers. Watch at your own discretion):
http://conformis.orlive.com/videos/the-conformis-itotal-g2-patient-specific-kneereplacement-
system
For more information on ConforMIS personalized total knee replacement you can download the following brochures or visit www.myconformisknee.com:
English:
Comparison Personalized versus Traditional Total Knee: http://origin.library.constantcontact.com/download/get/file/1111349463869-
392/ConforMIS+vs.+Off-the-shelf+Implants.pdf
General Info: http://library.constantcontact.com/download/get/file/1111349463869-
109/MK02653AB_Patient_iTotal_Brochure.pdf
Frequently asked questions: http://library.constantcontact.com/download/get/file/1111349463869-
110/MK02654AB_iTotal_FAQ.pdf
Spanish:
Traditional Total Knee Replacement
For over 10 years in practice and 5 years of residency and fellowship, Dr. Martin has performed traditional total knee replacement with mostly excellent results. I always discuss traditional total knee replacement as an option with patients because it is the most time tested procedure for the knee. Many cases with significant deformities, ligament injuries, knees with prior surgery, etc. are not candidates for personalized knee procedures and traditional total knee replacement is the only reasonable option.
Although the procedure helps most people, the main issue I have with total knee replacement is that approximately 1 in 5 patients who undergoes the procedure is not satisfied with their outcome. That does not mean, in most cases, that the patients are not better off than they would have been without it (although that is possible with any surgery). It just means they are typically not as happy with the procedure as they thought they would be.
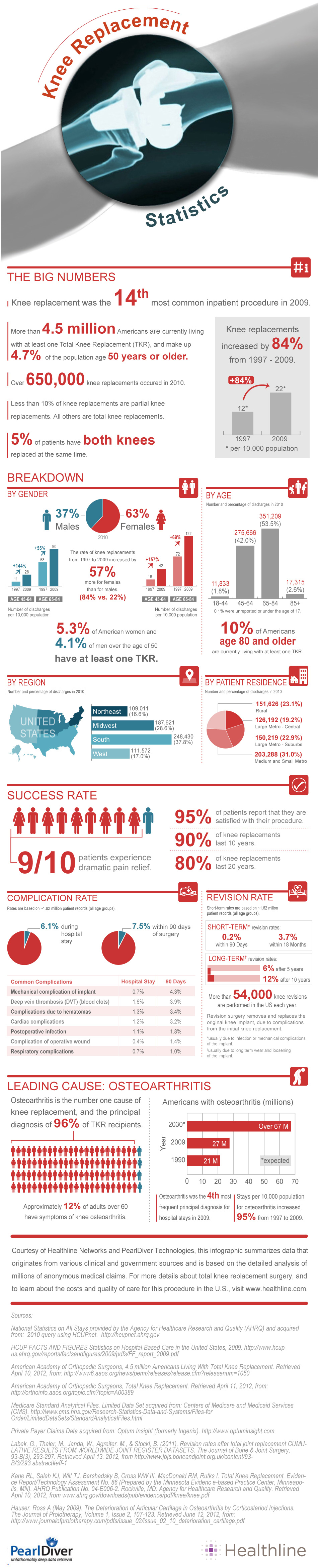
For an excellent review of statistics regarding total knee replacement, see the following infographic (the one statistic I don’t agree with is their satisfaction statistic (see the review in the Personalized Knee Section for this data):
SOURCE: http://www.healthline.com/health/total-knee-replacement-surgery/statisticsinfographic
When it comes to choices of implants, Dr. Martin tends to utilize the Depuy Sigma system, which was invented by his Mentors Dr. Thomas Thornhill and Dr. Richard Scott at the Brigham and Women’s Hospital and Harvard Medical School. This is one of the most widely used implants in the world, with an excellent track record for longevity.
Figure 5. Picture and X-ray of Depuy Sigma Rotating Platform Total Knee

For more information visit the Depuy/Johnson & Johnson website
www.kneereplacement.com or download the following brochures:
English: http://patients.depuyorthopaedics.com/binary/org/DEPUY/doc/pt.com/0609-46-000r11_TKR_final.pdf
Spanish: http://patients.depuyorthopaedics.com/binary/org/DEPUY/doc/pt.com/0610-75-000r5.pdf
For comprehensive information on total knee replacement from the American Academy of Orthopedic Surgeons visit: http://orthoinfo.aaos.org/topic.cfm?topic=A00389
Revision Total Knee Replacement
Dr. Martin has special expertise in performing surgery on knee implants that have failed. This is called Revision Knee Replacement and is required generally due to:
- Loosening of implants/Mechanical failure
- Infection
- Instablity
- Wear of the polyethylene liner
- Persistent Pain
- Stiffness
- Fractures around the implants
- Patella (knee cap) problems
- Other issues
Dr. Martin co-authored the section on Complications of total knee arthroplasty in UpToDate® which is utilized worldwide. To read this professional level material, visit: http://www.uptodate.com/contents/complications-of-total-kneearthroplasty
Although, rare complications and reoperations can and do occur. Close to sixty thousand reoperations on total knees occur each year in the United States. Studies have demonstrated approximately 6% of knees have required reoperation within the first five years and 12% within the first 10 years (what this also means is that close to 90% of total knees done today will last 10 years or more).
Generally, revision total knee replacement is a higher risk operation, as the tissues have already be disrupted. Implants with stems and devices to obtain better fixation are typically utilized.
Figure 6. Picture and X-ray of revision total knee components.

For more information on revision surgery from the American Academy of Orthopaedic Surgeons visit: http://orthoinfo.aaos.org/topic.cfm?topic=A00510
SHARED DECISION MAKING MODULES:
This information is coming soon